

Sponsored content by Coloplast Canada.
We care about your health and well-being and we want to let you know about an important change to Canadian clinical recommendations for intermittent catheter use. As of 2020, Canadian nurses no longer support the re-use of intermittent catheters.1Instead, Canadian urologists and nurses recommend single use intermittent catheters, ideally those that are hydrophilic or pre-lubricated.

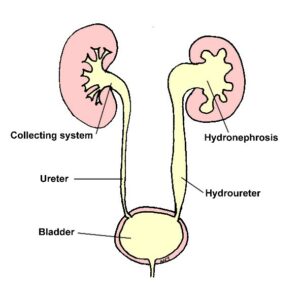
UTIs are a constant concern for catheter users. The new Canadian recommendations for catheter use recognize this, and work to help Canadian catheter users keep their bladder healthy.
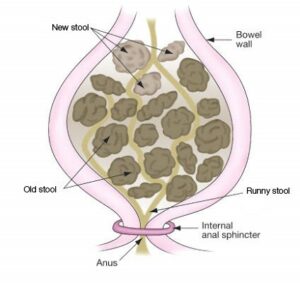
Re-using intermittent catheters causes unnecessary bacteria contamination, which may result in urinary tract infections
(UTIs).
Single-use hydrophilic or pre-lubricated catheters are recommended because they appear to lower the risk of UTI, may result in less urethral trauma, and have a higher convenience and ease of use compared to conventional uncoated catheters.
Need help with coverage? Product reimbursement in your province can be complex and overwhelming. Coloplast’s new Reimbursement Specialist offers expert guidance on insurance coverage, claims, and eligibility to ensure you get the personalized support you need.
For more information, please contact us at 905-829-7665 or at [email protected] Monday-Friday 9am-5pm ET
*findings not specific to Coloplast catheters
Clean Intermittent Urethral Catheterization in Adults – Canadian Best Practice Recommendations for Nurses. Developed by Nurses Specialized in Wound, stomy and Continence Canada, Canadian Nurse Continence Advisors, Urology Nurses of Canada, and Infection Prevention and Control.1st Ed. 2020.
Can Urol Assoc J 2020;14(7):E281-9. http://dx.doi.org/10.5489/cuaj.6697
Coloplast Market Study_IC Research_2015_Data on file
Bogaert GA, Goeman L, de Ridder D, Wevers M, Ivens J, Schuermans A. The physical and antimicrobial effects of microwave heating and alcohol immersion on catheters that are reused forclean intermittent catheerisartion. Eur Urol. 2004;46(5):641-6
Chan JL, Cooney TE, Schober JM. Adequacy of sanitization and storage of catheters for intermittent use after washing and microwave sterilization. J Urol. 2009;182(4 Suppl):2085-9

Les urologues et le personnel infirmiercanadiensrecommandentplutôtl’usage unique des cathétersintermittents, spécifiquement les cathéters à revêtement hydrophile ou prélubrifiés.
Les IVUsontunepréoccupationconstante pour bon nombred’utilisateurs et d’utilisatrices de cathéters. Les nouvellesrecommandationscanadiennes relatives à l’utilisation des cathétersentiennentcompte et sont revues pour aider les utilisateurscanadiens à maintenir la santé de leurvessie.
La réutilisation des cathétersintermittentsentraîne des risques de contamination bactériologique, ce qui peut causer des infections des voiesurinaires (IVU).
Les cathéters hydrophiles à usage unique ouprélubrifiéssontrecommandés, parcequ’ilssemblentréduire les risquesd’IVU, éviter les dommagesurétraux et s’avèrent plus pratiques et faciles à utiliserencomparaison avec les cathétersclassiques non lubrifiés.*
Besoin d’aide en matière d’assurance? Le processus de remboursement de produits de votre province peut s’avérer fastidieux et compliqué. Chez Coloplast, notre spécialiste en remboursement offre des conseils avisés sur la couverture d’assurance, les réclamations et l’admissibilité pour assurer que vous obtenez le soutien dont vous avez besoin. N’hésitez pas à communiquer avec nous par téléphone au numéro sans frais 1 (905) 829-7665 ou par courriel à l’adresse ca_reimbursement@coloplast.com du lundi au vendredi de 9 h à 17 h (HNE)
*Résultats non spécifiques aux cathéters de Coloplast.
Clean Intermittent Urethral Catheterization in Adults – Canadian Best Practice Recommendations for Nurses. Developed by Nurses Specialized in Wound, stomy and Continence Canada, Canadian Nurse Continence Advisors, Urology Nurses of Canada, and Infection Prevention and Control.1st Ed. 2020.
Can Urol Assoc J 2020;14(7):E281-9. http://dx.doi.org/10.5489/cuaj.6697
Coloplast Market Study_IC Research_2015_Données consignées.
Bogaert GA, Goeman L, de Ridder D, Wevers M, Ivens J, Schuermans A. The physical and antimicrobial effects of microwave heating and alcohol immersion on catheters that are reused forclean intermittent catheterisartion. Eur Urol. 2004;46(5):641-6.
Chan JL, Cooney TE, Schober JM. Adequacy of sanitization and storage of catheters for intermittent use after washing and microwave sterilization. J Urol. 2009;182(4):2085-9.